Assessing behavioural change post-head injury and impact on return to work

Dr John McMahon, Neuropsychologist at MedicoLegal Specialists, discusses the assessment of behavioural change following head injury and, how it might impact the patient’s return to work, with a focus on psychometric assessment. Dr McMahon gave a seminar presentation on this topic for Legalwise Seminars. Click here for our June Psychological and Psychiatric Injury Conference series.
Psychological injury:
- Is harm represented by an abnormal mental state.
- Such injuries are abnormal mental states that causes significant impairment in social, occupational or other functioning.
Stress:
- Is a state of physiological or psychological response to internal or external demands.
- Involves changes affecting nearly every system in the body to meet the demands, and changes range from increased skin conductance to, heart palpitations, sweating, dry mouth, shortness of breath, fidgeting, faster speech, and gross motor movement are potentiated. Stress is a normal part of life.
Strain:
- is the physical consequences of stress.g. jogger’s knee.
- Mental disorder is an incidence of strain through changes in either:
- Neurochemical functioning
- Brain Changes
- Brain Damage
- In PTSD and Major Depressive Disorder there are changes in the hippocampus and amygdala that can be measured post mortem.
Common Diagnoses that represent psychological injury:
- Mild to Moderate Range:
- Adjustment Disorder with Anxiety
- Adjustment Disorder with Depressed Mood
- Adjustment Disorder with Mixed Anxiety & Depressed Mood
- Adjustment Disorder with Disturbance of Conduct
- Severe Range :
- Post-Traumatic Stress Disorder
- Major Depressive Disorder
- Common Diagnoses that complicate response to physical trauma:
- Chronic Pain Disorder with Psychological Factors
- Somatoform Disorder
- Factitious Disorder
Common Diagnoses due to traumatic brain injury:
-
- Mild Neurocognitive Disorder due to Brain Injury with/without behavioural disturbance
- Major Neurocognitive Disorder due to Brain Injury with/without behavioural disturbance.
- “Major” means “Substantial impairment of cognitive performance preferably documented by standardized neuropsychological testing or, in its absence, another quantified clinical assessment.” The cognitive deficits interfere with independence in everyday activities, such as paying bills or managing medications.
- Minor: “A modest cognitive decline from previous level of performance in domains such as complex attention, executive function, learning and memory, language, perceptual motor, or social cognition”.
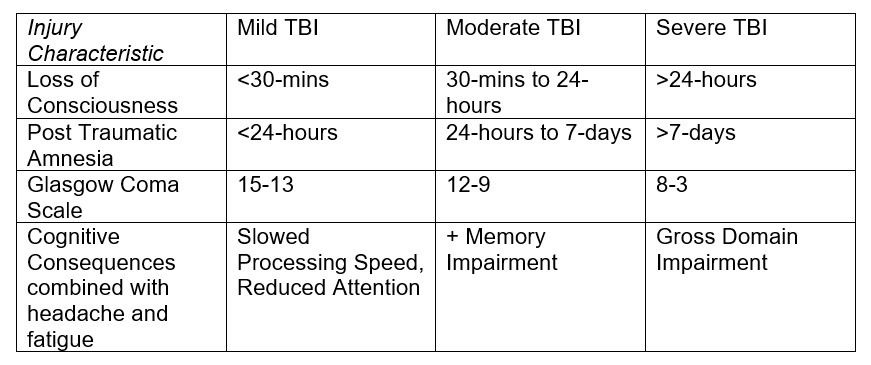
Common complications due to traumatic brain injury (TBI):
- The recovery from brain injury takes 18-months to 2-years, with subtle improvements up to 5-years post injury. Usually these latter changes are adaptation rather than continued recovery of the brain.
- Headache and fatigue are the most common symptoms that disrupt daily functioning.
Typical Neuropsychological Test Battery:
- Interview (1-hour)
- Symptom Validity Testing (TOMM etc)
- Wechsler Adult Intelligence Scale (1–2 hours)
- Wechsler Memory Scale (1-1.5 hours)
- Tests of Executive Functioning (D-KEFS 1.5-hours)
- Questionnaire (MMPI-2, MMPI-2-RF, PAI, Ruff NBI: 0.5 – 2-hours)
Neuropsychological Testing:
- Is a direct observation of pace, persistence and cognitive capacity enduring for 4- to 8-hours.
- Provides a standardized measure of performance in specific domains which permits mapping of assistance to the individuals deficits and programming of restrictions to avoid further harm.
- Allows fine grained identification of barriers to recovery and function.
Dr John McMahon has a Bachelor of Psychology (Honours) and Doctor of Psychology (Clinical) degrees, and commenced working in psychosocial rehabilitation of people with traumatic brain injuries and neurological conditions in 1997. He was a senior consultant to a pain management program from 2005 to 2007. He has testified in magistrates, district and supreme courts in NSW, ACT and Victoria in criminal and personal injury matters. He has presented nationally and internationally on the topics of executive functioning, the frontal lobes of the brain, and malingering. He is trained in the assessment of permanent impairment. He was a WorkCover Independent Consultant for 5-years on the originating panel and MAS Assessor in NSW and an independent examiner for Transport Accident Commission and WorkSafe in Victoria. He a partner in, and the Chief Scientific Officer for, Navigator Group managing and researching programs for the Active Recovery Clinics, MedicoLegal Specialists, Navigator Health and Oncall Advisor.
Active Recovery Clinics treat compensable injuries including whiplash, shoulder, knee and hip injuries and primary psychological injuries using an at home physiotherapy treatment and monitoring system SWORD Phoenix and the psychological therapy Eye Movement Desensitization and Reprocessing Therapy. Medico Legal Specialists is a national medicolegal and forensic consultancy with a panel of over 350-medical specialists. Navigator Health is a national absenteeism program and independent support services for people with compensable injuries and currently supports over 2000 people under worker’s compensation and CTP schemes. Oncall Advisor is a virtual Chief Medical Officer service with a case management consultation platform and telephone access to medical experts. Dr McMahon is currently writing a PhD in the Faculty Of Health and Medicine at University of Sydney “Psychological Injury: A Quantitative Assessment of Natural Justice and The Optimum Management of Psychological Factors in Compensation Systems”. Connect with Dr McMahon via LinkedIn ![]() .
.